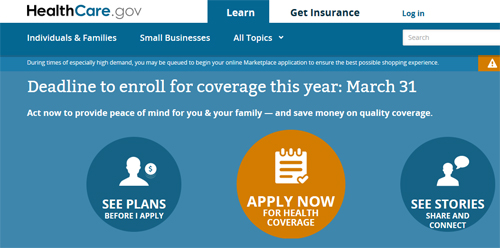
Open enrollment deadline is March 31
- If you submit your application for healthcare coverage March 16 through March 31, your effective dates of coverage would either be April 15 and May 1
Triggering events are:
- A qualified individual and any dependents losing other minimum essential coverage which include: loss of Medicaid and CHIP–as a result of a reported
- change in household income, or as a result of other circumstances
- A qualified individual gaining or becoming a dependent through marriage, birth, adoption, or placement for adoption
- An individual, not previously lawfully present, gaining status as a citizen, national, or lawfully present individual in the U.S
- Consistent with the Medicare Prescription Drug Program, a qualified individual experiencing an error in enrollment
- An individual enrolled in a QHP adequately demonstrating to the Exchange that the QHP in which he or she is enrolled substantially violated a material provision of its contract
- An individual becoming newly eligible or newly ineligible for advance payments of the premium tax credit or experiencing a change in eligibility for cost-sharing reductions (does not apply if they become eligible for an increase or decrease in their existing advance payments of the premium tax credit; however if an individual experiences a change in his or her existing payments of the premium tax credit in tandem with a change in level of cost-sharing reductions, the individual could qualify for this special enrollment period)
- New QHPs offered through the Exchange becoming available to a qualified individual or enrollee as a result of a permanent move (includes Qualified individuals newly released from incarceration)
- The individual is an Indian, as defined by the Indian Health Care Improvement Act.
- A qualified individual or enrollee meeting other exceptional circumstances, as determined by the Exchange or HHS.
Even after this open-enrollment period passes, we can still offer you Short Term Medical insurance and other supplemental health insurance medical products outside the open enrollment period.
>>> Minimum essential coverage — what you need to know
Most Americans must now have health insurance coverage that is minimum essential coverage (MEC). If insured’s do not have MEC, they may be subject to payment of a penalty. Here at Benton White Insurance, I offer plans that qualify as MEC. We offer non-MEC plans also mentioned above (Short Term Medical insurance and other supplemental health insurance medical products). We will advise you in our discussion more about MEC and outline the program you need as being either MEC qualified or non-MEC and the possible consequences of purchasing a plan that is not MEC.
There is an enormous amount of information that we all have to learn in order to make a qualified decision about healthcare coverage these days. We’ll do our best here at the insurance agency to help you in any way that we can and if we don’t have the answers, we can certainly get them for you. We want you to be covered and have choices that you are currently available to you. However, after March 31, the options are much more limited. Please contact me personally if I can help either by EMAIL – Benton@BentonWhite.com or 615.377.1212





